
(image: Glamour UK)
Here it is, my
GLAMOUR UK article on being a curvy or plus size bride.

(image: Glamour UK)
Here it is, my
GLAMOUR UK article on being a curvy or plus size bride.
(image: GoThinkBig)
On Monday, I returned from a wonderful holiday to Israel with my fiance Rob, seeing friends and family. I hadn’t been to Israel in 9 years for various reasons and he hadn’t been for 13 years (!) so we were determined to make the most of our trip. We definitely don’t want to leave it so long next time.
We travelled around the country staying with family and in hotels too. If anything, we almost packed in too much trying to see everyone- and I still didn’t get to see everyone I wanted to as we were only there for a week. I was also very conscious of the fact that it was very hot and it became apparent that I couldn’t cope with walking in 36 degree heat for too long!
I made sure that I had lots of water on me as my medication, Lithium, dehydrates my body quickly so I have to intake more water than most. I found that through heat and dehydration, I would get tired quite quickly so if we had spent a morning travelling, I would need to spend a few hours either resting in air conditioning or sleeping.
In general, my anxiety is better when I am abroad, though there were a few days where morning anxiety did overwhelm and I chose to rest and sleep and then go out later in the day. My fiance was very understanding of this and went for a wander some mornings. However, once I was rested and had eaten breakfast/ drunk lots of water, I was able to enjoy and do lots of fun things.
On our trip we went to visit my best friend/ cousin and her family in a place called Tel Mond, near Netanya and we went for a day trip to Netanya- which is a beach side resort. They also made a barbeque for us when we arrived which was lovely and we saw other friends who live there. We met their newest arrival – gorgeous baby girl- and I had lots of cuddles with my new cousin!
We then went to Jerusalem for a few days- to the Western Wall to pray, walking in the Old City, seeing my other cousins and catching up over ice cream and meeting friends for dinner in the evening. We spent time in the Jerusalem First station near our hotel, which has restaurants and stalls as well as live music- a bit like Covent Garden! Rob and I went shopping and bought things for our future home as well as for family in England.
After this, we travelled to spend Jewish sabbath- shabbat with my other cousins who moved to Israel last year- and spent time walking around where they live and meeting their friends. It was restful and lovely to catch up with them, eat delicious food and rest.
Our final day was spent in Tel Aviv, going in the swimming pool, walking around the streets by the beach, drinking iced coffee and going out for dinner with another cousin who happened to be travelling there with her friends. Rob and I also had time to ourselves which was important and we didn’t want to leave!
I am lucky that my medication very much helps my bipolar and so I was able to do all of the above.
For me when abroad, my main concerns are taking my medication on time and each day, getting enough sleep, eat well, staying out the sun at hot times and making sure I rest and drink enough. If I follow that, I can largely function.
Sometimes my anxiety about being in a new place can kick in upon waking- so I was thankful my fiance understood it took me a bit longer to adjust to the day, but once I was rested, I was able to really enjoy the holiday.
Its important to note that everyone is different on holiday. However, it is vital to cut yourself slack, take rest days (or rest half days) and also take medication on time. I don’t drink alcohol on my meds- but keeping hydrated if you are is so important too.
Also make sure you declare your condition on travel insurance so you are covered if you become unwell abroad! This will make it more expensive but worth it. You don’t want to get sick abroad and have no cover.
I am pleased too that I stayed well- despite being very tired on my return. I made sure I caught up on sleep and didn’t go straight in to work – although I am now back at work.
I am missing my trip already and so thankful to my fiance, friends and family for making it so special.
Mood disorders encompass many disorders of how you feel from day-to-day, whether that is abnormally elevated (mania) or depressed and in low mood. They can include depressive illness such as major depressive disorder, dysthymia, postnatal depression and the bipolar spectrum disorders. They also feature anxiety and panic disorders. These are often down to brain chemistry and sometimes environment.
(image: Pinterest/ Healthyplace.com)
Major Depressive Disorder
Major depression is defined as a depressive illness where you experience a significantly lowered mood and a loss of interest in activities that you would normally enjoy. While it is normal to feel sadness and grief when your life significantly changes, such as when a loved one passes away, when it doesn’t go away or gets worse, it may evolve into major depression. Some of the symptoms of depression are:
• Feelings of helplessness or hopelessness • Feeling guilty over insignificant things • Withdrawing from family and friends • Drinking alcohol or taking drugs as a coping mechanism • Having problems with concentration • Being unproductive • Having a lack of confidence • Feeling irritated or frustrated • Having a lack of interest in sex.
While sometimes a depressive episode seems to come out of the blue, there are often things that can trigger them. These may include: Genetic risk factors • Alcohol or other substance abuse • Medical problems such as thyroid issues or chronic pain • Certain medications such as steroids • Sleeping problems • Stressful life events
Studies have shown that there appears to be a genetic component to depression. That is, if one of your parents has a depressive illness, you may end up suffering from depression yourself.
Dysthymia is a chronic form of depression that occurs when you suffer from a mild to moderate depression for at least two years. Although dysthymia causes problems in everyday life, dysthymia is often not severe enough to warrant hospitalisation. The chronic nature of the disorder means that you may believe that you have always felt like this.
The good news is that there are a wide range of medications to treat major depressive disorder, such as antidepressants. There are many kinds of medications around, and you may have to try a few until you and your psychiatrist find the perfect one with little to no side effects.
As of the time of writing, the antidepressants most commonly used are SSRIs and SNRIs (selective serotonin reuptake inhibitors and serotonin-norepinephrine reuptake inhibitors). These refer to the types of neurotransmitters (chemicals in the brain that affect mood, among other things) that they affect.
With antidepressants, it is extremely important not to stop medication all at once, unless there are serious side effects and even then, only under medical advice. This is because of discontinuation syndrome. Simply put, this means that your body gets used to the medication being in your system (different to addiction where you crave the drug) and you experience symptoms such as nausea, dizziness and insomnia, to name a few.
Another important way to treat depression is psychotherapy in one form or another. This can help you by learning coping skills to deal with depressive thoughts and negative thinking, as well as having someone to speak to with complete privacy. There are a few other ways for you to combat depression in adjunct to medications or therapy.
These are: • Maintaining good sleeping habits • Exercising more • Seeking out activities that bring you pleasure • Being around caring and supportive people
Postnatal Depression
Postnatal depression is a depressive illness where a new mother experiences depression in the first few months after giving birth to a child.
Some of the symptoms of postnatal depression include:
• Feeling sad or empty • Lowered self-esteem • Changing appetite (usually a decrease) • A loss of enjoyment in everyday activities • Changes in sleep patterns such as insomnia • Not being able to concentrate • Feeling cut off from the baby • A loss of interest in sex • Feeling ashamed, guilty or inadequate • Withdrawing from family and friends • Mood swings • Thoughts of harming yourself or the baby
There are a number of factors that make postnatal depression more likely. Some of these may include: • A history of depression, especially postnatal depression in the past • If the baby is sick or colicky • If you are in an abusive relationship • If you are suffering from stress • If you have little support from family and friends •
Treatment for postnatal depression is essentially similar to that for major depression, such as antidepressants and therapy and in some cases intervention from a psychiatrist or hospital team is required.
Bipolar Disorder Spectrum
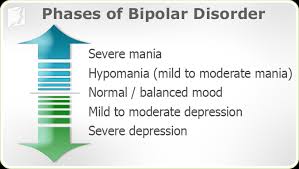
Bipolar disorder is a mental illness characterised by periods of extreme mood states known as mania and depression. It is one of the most serious mental illnesses and is the sixth most disabling condition in the world at the time of writing. It is chronic and potentially life threatening. However, those with it can go on to recovery and live happy and fulfilled lives between episodes.
According to some studies, one in fifty people may suffer from a form of bipolar disorder. In many cases, there is a family history.
Mania is one pole of bipolar disorder – an extremely elevated or depressed mood, sometimes accompanied by psychosis. You may have racing thoughts or speak so quickly it is difficult for others to understand. You may also have trouble getting to sleep at night or suffer from insomnia. There is a danger of reckless behaviour such as overspending, unsafe sexual activity or aggression. You may feel a sense of grandiosity, making unrealistic plans. Despite mania feeling great at the time, the consequences of mania can be destructive.
Some of the signs of depression include a lowered mood, self-esteem or interest in enjoyable activities, pessimism, reduced energy and changes in appetite. Suicidal thoughts are also possible and must be monitored closely. As bipolar disorder is a recurrent illness and there isn’t any known cure, you may need to take medications to maintain your mood at a normal level.
Hypomania is the hallmark of bipolar II where the patient might feel euphoria or agitation. Hypomanic episodes are similar to manic episodes except they are less severe and sometimes pleasurable to you. There is never psychosis in a hypomanic episode. Despite hypomania increasing productivity, or making you feel increased self-esteem, the consequences can be major, especially as your mood goes down to depression.
A mixed state is a combination of manic and depressed symptoms. In a mixed state you may feel very sad or hopeless while feeling extremely energised. These can be dangerous, because of the suicide risk from being depressed as well as impulsive. If you feel you are heading into a mixed state, you should contact your psychiatrist as soon as possible.
Bipolar disorder type I is characterised by at least one episode of full-blown mania as well as depressive episodes. There is also a chance of psychosis (delusions/ hallucinations) accompanying a manic episode. Bipolar type II features only hypomania and never mania or psychosis. While these manias are less destructive, the depression tends to be worse, and there is often a high suicide risk.
Cyclothymia is a bipolar spectrum disorder where you may have long periods of minor depression lasting at least two years alternating with hypomania. These depressive periods tend to be irritable and agitated rather than melancholic and lacking in energy.
Bipolar NOS (not otherwise specified) simply refers to bipolar disorders that do not strictly meet the criteria of any of the previously mentioned types of bipolar disorder.
The treatment of bipolar disorder involves medications such as Lithium carbonate, lamotrigine, sodium valporate, and quetiapine, as well as psychotherapy to help overcome negative thoughts that exacerbate depression or after effects of mania.
As bipolar disorder is a recurrent illness and there isn’t any known cure, you may need to take medications for life to maintain your mood at a normal level. Despite this, many patients continue to do well as long as they stay compliant with treatment and keep aware of their changing mood states.
(image: MTVFORA: http://fora.mtv.ca/words-of-wisdom-celebrity-quotes-on-mental-wellness/)
Anxiety Disorders
The term anxiety disorder covers a wide range of illnesses from panic disorder to post-traumatic stress disorder (PTSD). Despite the wide range of diseases, many share similar treatment options. There is a stigma affecting some anxiety disorders due to stereotypes in the media.
Generalised Anxiety Disorder
It is normal for people to feel some anxiety over normal life events such as exams, work problems or family issues. However, when it causes problems in your everyday life or is particularly severe you may have an anxiety disorder. Generalised anxiety disorder involves having irrational fears, such as being afraid harm will come to you or your loved ones, financial issues, health, relationships and work.
Physical symptoms when experiencing anxiety may include: • Light-headedness • Becoming tired easily, or being unable to sleep properly • Feeling tense or restless, or losing your temper easily • Nausea • Shortness of breath • Headaches • Trembling • Muscle tension Treatment generally involves medications or therapy.
Psychological treatments may involve: • Learning relaxation techniques such as muscle relaxing exercises or meditation • Therapy to teach you how to solve problems that cause anxiety with anxiety disorders, psychological treatments are generally more effective than medication, however it can still be useful.
The most common treatments are antidepressants or benzodiazepines such as alprazolam or diazepam. Generally, benzodiazepines shouldn’t be taken long-term, as there is a risk of becoming dependent on them.
Anxiety disorders are relatively common in the population, with statistics that approximately 25% of the people suffer some kind of anxiety disorder that may warrant treatment in their lifetime. Anxiety is treatable, and therapy or medication may minimise the effects on your life and relationships.
Panic Disorder
Panic disorder is a mental health condition where you experience a feeling known as a panic attack recurrently.
Some of the symptoms of a panic attack include: • Shortness of breath • Dizziness or light-headedness • Tightness or pain in the chest • Trembling or shaking • Dry mouth • Muscle tension • Difficulty gathering thoughts or speaking • Tingling fingers or feet • A choking or smothering feeling • Hot or cold flushes • Nausea or butterflies • Blurred vision • Fear of dying, losing control or going mad
When you have panic disorder, you may also worry about the implications of a panic attack such as humiliation or feeling of going crazy.
You may try and flee from the situation hoping the panic attack will stop. Panic disorder is generally treated via therapeutic methods rather than medications. This may involve your doctor teaching you about panic disorder, for example, that a panic attack is distinguishable from other mental illnesses such as other anxiety disorders or psychosis – this is known as psycho education.
A therapist may instruct you not to avoid any situations where a panic attack may occur. This may be unpleasant at first, but slowly you will not feel anxious in the situation. This will help prevent agoraphobia and the disability it causes.
A common treatment for anxiety disorders is CBT – but there are many types too including exposure therapy and talking therapies. They can be incredibly helpful for you to overcome feelings of anxiety.
This guest blog was written by Ellie Willis, an expert in mental health.
When most people think of bipolar disorder, they may think of the two opposing poles that make up the illness. High and low. Manic and depressed. Many also believe that all people with bipolar flit between these moods constantly and that the illness is severe or alike in everyone who has it. This is not the case.
There are two types of bipolar disorder. I have the first one – Bipolar affective One disorder, which means that I have serious manic episodes which include psychosis (loss of touch with reality). This has happened to me twice in my life and both times I have needed hospitalisation. Bipolar two is characterised by lesser manic episodes (hypomania) and more mixed states.
(image: https://www.34-menopause-symptoms.com/mood-swings.htm)
Being Bipolar One is very challenging. When I get ill, I get really really sick. Loss of insight, loss of reality, needing anti psychotic medicines now- ill. Ill to the point of being sectioned under the mental health act due to lack judgement and insight. Believing that my family are out to get me and people are going to harm me – ill. Really unwell.
When one of these serious manic episodes strikes for me, my thoughts begin racing and I can’t concentrate. I don’t sleep, I am more creative in the short term but a gibbering wreck in the long term. I start believing I can do things that I can’t rationally. I am super vulnerable and I speak much faster. I may not make much sense and when the delusions begin, I start believing I am going to be harmed.
Luckily, these episodes are kept at bay by a host of excellent medications including Lithium and Quetaipine. I also take anti depressants to keep the low periods at bay in my life.
Full blown psychosis and mania for me are very rare but they do happen. In 10 years, from 2004-2014 I did not have a hospitalisation. I was depressed and anxious but I was able to recover at home.
I had no hypomanic or manic episodes for a decade! No psychosis. One therapist even questioned my diagnosis, before my 2014 hospitalisation.
Mania for me means danger. That danger means I am more vulnerable. I have to be very careful who I surround myself with during those times. I don’t drink alcohol to excess or take drugs, but some with this kind of mania do. Or they spend lots of money or engage in risk taking behaviours such as sexual activity.
I have learnt that as long as I take my medication regularly, get enough sleep, eat well (and don’t engage in long haul travel) that I can keep my symptoms at bay. If my medicines work! (this is always a fear.. that they could stop working).
Mania for me strikes out of the blue sometimes. I also have to be careful that my mood stabiliser medicine is holding me- as with high doses of anti depressants, mania can be triggered without it.
When in psychosis in hospital I have thought the following untrue delusions
– I am being harmed by my family
– There are CCTV cameras watching and filming me in my bedroom/ hospital room
– I have been abused in some way (my mind convinces itself)
– I am being held by a criminal gang (in hospital)
These delusions have always disappeared over time, with excellent care from psychiatrists and psychologists, anti psychotic medicine and good support from family.
I don’t get these when well, and rarely have to go through them. I am learning to accept that my brain chemistry is not the same as other people and having bipolar, a chronic illness, is not my fault. I just do the best I can to manage symptoms and keep myself as well as possible.
If you want to share your story of mania and bipolar, please do write below.
There is hope and recovery after mania. Thank you to all on the Facebook group who voted for this one.
Love, Eleanor x

(image: healthyplace.com)
I havnt written a blog update on life for a while. I think this is because so many amazing and exciting things have been happening that the anxiety and panic attacks have had less air time.
Many of you know that since January, I have been published widely across the media and am now writing as a career. Ive been nominated for a blog award, given my first radio interview, am writing chapters for a potential book and achieved my dream of being featured in Glamour Magazine, Cosmopolitan and Elle as well as being a writer for Metro, Happiful Magazine and the Jewish News where my life story was published. And working with charities such as Mind, No Panic, SANE and STOP Suicide and the amazing team at AND Digital.
And breathe.
This is all exciting and wonderful and I feel very blessed that people are accepting of me and my story. I feel lucky to have a new career and to be achieving my dreams.
But what most of you may not see or know is I still suffer with social anxiety.
I was invited to record a mental health podcast but couldnt travel there because it felt too overwhelming to step into this new big media environment. I was due to give a talk but couldnt attend due to anxiety about standing up there on my own being vulnerable. Luckily we had planned for this scenario and they were so kind and used my blog testimony anyway.
However I hate letting anyone down. For me panic attacks happen as a response to stress. I get triggered in new work situations and when I havnt met the person before. Everything feels overwhelming and all I want to do is hide from the fear.
Ive been in therapy for 6 months…psychodynamic …talking therapy and its been helpful. Im still learning to find coping mechanisms as my response to the feared situation is often to cancel or postpone it and shut down.
Im learning how to navigate my new world whilst having a panic disorder. I will get negative thoughts and fears, tight chest, racing heart. And then have to stop the feared trigger.
I know I am not the only one feeling like this and many of you also have anxiety disorders. Please know that you aren’t alone.
Seek support from your doctor and try different methods. I find meditation to be helpful to me alongside exposure therapy and talking therapy. It will be trial and error for you as it is for me.
Im not sure if i should have anxiety medication for emergencies as I already take so much medication. But it could be that I need them in order to function and progress further. Im on anti depressants and mood stabilisers already which help me.
I feel lucky to be able to work and write and blog. I just hope that I can learn to cope better in face to face work situations too. Thanks to all who voted for this blog on Facebook and I hope it will give you an insight.
Eleanor x
I was so excited to be featured in Olivia Blair’s article for Cosmopolitan UK on anti depressants- 6 women share what its really like to be on Anti depressants.
I am so thrilled to be in this article with 4 other brave women. My first time in Cosmo! Thank you Olivia.
Below is my part of the article but please click here to read the others experiences too: https://www.cosmopolitan.com/uk/body/health/a18720313/women-on-antidepressants-working/

(image: Getty Images/ Cosmopolitan)
I become suicidal when depressed, it’s vital I take medication for my health”
Eleanor Segall, 29, mental health blogger
“I started taking antidepressants when I was 15 after an acute depressive episode where I had to take time off school. A year later I was diagnosed with bipolar disorder and was hospitalised so I was prescribed a mood stabiliser as well to keep me on an even keel.
I was concerned about some of the side effects but the positives for my mind and brain chemistry outweighed the negatives. Over the years, I have been on different antidepressants including fluoxetine, duloxetine and now sertraline. I also continue to have psychodynamic therapy and have tried CBT, art therapy and meditation.
There is a big stigma around anti depressants, particularly against bipolar and other chronic conditions. But I think this new study offers proof that, for some of us, they are vital.”
(image: amyransom.com)
I wasnt going to write a blog on this because it might feed the Twitter trolls. But I have decided that its really important that I speak out about whats been going on this week on there, in realm of mental health on social media. Theres been a lot of stigma against medication as well as much support for it.
This week, a study by Oxford University and published in the psychology medical journal the Lancet, found that anti depressants work and are effective in a large number of cases. It was hailed as the first major study to prove this. Some medications were found to be more effective than others, but it provided a fantastic proof- that anti depressant medications do help relieve depression in many cases. They are not just a placebo pill.
However, of course, there are a large number of people who have had bad experiences with anti depressants and want to make their voices heard- yet often at the expense of those of us who it works for.
On Twitter, using the trending hasthtag #antidepressants and #medsworkedforme, I shared that anti depressants coupled with my mood stabilisers, have very much helped my bipolar disorder. My brain chemistry and illness is such that unmedicated I can have episodes of suicidal depression, psychosis and mania. My medication keeps my moods balanced and well, so I can function and live a normal life. I have been on anti depressants for almost 15 years now. I have been on fluoxetine, duloxetine and now sertraline.
The only bad experience I ever had with them is when my previous mood stabiliser stopped working and due to an increased dose of duloxetine to relieve my depression (which it did), I tipped over into a fast and unpredictable manic episode. This is the risk that those of us with bipolar run.
Yet, by and large my experiences with meds have been hugely positive. They keep me stable and well.
Unfortunately, on Twitter, I got trolled for the first time by people sharing the following ‘helpful’ opinions (they were not helpful and highly stigmatised):
1) You should reduce your sugar intake as sugar causes highs and lows and is addictive as cocaine. If you reduce your sugar, your bipolar will improve.
(To this I had to reiterate that no medication and less sugar will make my illness worse… and that excess sugar does not cause bipolar 1 disorder.. i.e. it does not have that impact on my mood swings.. bipolar is a real illness in the brain. Reducing sugar may help with overall health but seriously you are going to tell me this?)
2) Others asked what alternative therapies I had tried- eg exercise instead of medication. I reiterated the above re psychosis and suicidal ideation. Which unfortunately cant be treated with exercise alone.
3) People shared their own stories eg the man who had multiple severe illnesses and takes no medication because ‘it shortens life span’ and its a medical fact apparently that these medications cause psychosis. (Some psychiatric meds cause side effects but psychosis- really? Also why would you tell me it will shorten my life?)
There was a lot of what I would call militant stigma against medication, either by people who fear it or have experienced negative effects.
While medication is not for everyone, we shouldn’t be shaming people for taking it. I shouldn’t be shamed for keeping my brain healthy and well through taking meds. And neither should any of you.
Make sure you fight this stigma (and the block button is always useful).
Love,
Eleanor

This is an extract from an article our founder Eleanor Segall wrote for Metro.co.uk. To read the full article click here:
http://metro.co.uk/2018/02/21/how-to-improve-on-screen-depictions-of-mental-illness-7315828/
As someone with bipolar disorder, I am often intrigued by depictions of mental illness on TV and film. For many years, mental illness has been stigmatised, and this has been reflected on screen. Thankfully, this stigma is beginning to be broken down, but it is still present.
In her award-winning article, Mental Illness in the Media, for the International Bipolar Foundation, Hosana Tagomori, who was a high school student when she worked on the piece, wrote: ‘The media often portrays characters with mental illness as incomprehensible, tortured and convoluted… the entertainment value often gets in the way of an accurate portrayal. ‘Patients are perceived as dangerous or insane, due to the inaccurate portrayals in media, where the character is almost always hopeless, deranged, and dangerous.’ ‘It is quite easy to subconsciously absorb these misconceptions.’
Indeed, this is a challenge that those of us with mental health issues face. We want our illnesses to be portrayed correctly and accurately on screen, without having to watch stereotypes. Depictions of mental health can be disappointing
Tagomori wrote: ‘In the television series Homeland, the bipolar character always seems to be the pop-eyed, insane mess who is constantly going ballistic: ranting, drinking and screaming’. While this can be true for some people with bipolar in the middle of a manic episode, it is not a balanced approach to the illness. We know that people with bipolar disorder can often be stable and well on medication and that a long time can elapse between episodes.
Portrayals of those with mental illness as ‘insane messes’ raises dangerous misconceptions, including that people with mental health problems will never get well. For me, a brilliant representation of bipolar disorder and postpartum psychosis appeared on EastEnders in 2015.
This centered around a story line for pregnant character Stacey Fowler (played by Lacey Turner), who has the disorder and experiences a psychotic episode after giving birth. Before watching the scenes in which Stacey has psychosis, I was concerned how it would be shown on screen, but I needn’t have worried. Sensitive, accurate portrayals of mental illness on screen can help to educate viewers EastEnders worked directly with the charities Mind and Bipolar UK to create the story line, so the script and performance were as accurate as possible.
In 2015, Dominic Treadwell Jones, producer of the story line spoke to the Radio Times, he said: ‘EastEnders have worked closely with Mind, Bipolar UK, other experts in the field and women with personal experience to show a story that is true and painful, while also filled with the usual twists and turns viewers have come to expect from EastEnders. Lacey is one of the most raw and intuitive actresses on TV.’
Also speaking to the Radio Times about the EastEnders story line, Clare Dolman, vice chair of Bipolar UK, said : ‘As the national charity supporting people with bipolar, we’ve been glad to work closely with the BBC on Stacey’s storyline. ‘There is a very high risk that women with bipolar will become ill when they have a child and 20-25% of them will have a postpartum psychosis, so it’s fantastic that EastEnders are raising awareness of this devastating condition.’
In the scenes where Stacey is experiencing psychosis, the character believes she is the Virgin Mary and that her baby is Jesus. She experiences delusions and auditory hallucinations. I was concerned about how I would feel watching it, but what I most felt was a sense of pride that British television was portraying bipolar correctly, sensitively and appropriately.
Twitter: https://twitter.com/MetroUK | Facebook: https://www.facebook.com/MetroUK/

(image: Pinterest)
The past few weeks have been incredibly busy- but exciting. This month has been a bit of a rebirth in many ways. My writing and blogging have truly taken off and been published in various different places- this month my story is in Happiful Magazine, two articles for Metro on mental health (www.metro.co.uk), I shared my story in the Jewish News here in the UK and online at STOP Suicide. It has been Time to Talk Day (about mental health), Childrens Mental Health Awareness Week and I have also volunteered this month with Jami (Jewish Association of Mental Illness) Mental Health Awareness Shabbat, which this year came to around 97 Jewish communities in the UK. I attended the panel event at a local community centre and discussion was had on mental health here in the UK, by experts including my friend Jonny Benjamin.
This month, I have also been asked by a friend to come in and talk to his work place about living with anxiety and what it means. So that is hugely exciting for me! I am also writing a mental health article for a top womens magazine- which is a dream of mine. I hope to share that with you when its published. I have been writing sample chapters for a book too and am in the limbo phase of waiting to hear what editors think.
So, its been a total whirlwind really as I have also been running my blog here and sharing peoples stories (and last month this blog was nominated as a finalist for a UK Blog Award). I was also asked last week if a social media editor could turn my story into a video for her 200 thousand followers so that is in process too. I had not ascertained how much interest there would be in my story.
Professionally, a lot is changing and I have to be very much aware to look after my mental health, to get enough sleep and rest, to make sure I take my tablets on time, to eat well and do some gentle exercise and to see and speak to my friends (and boyfriend of course). I have to keep grounded and rested in order to function effectively. Last week, the Jewish News article came out and I know it has had a positive ripple effect in my community- as my Mum was stopped in the pharmacy for people to talk to her about it. So thats exciting.
I am a shy person at heart and I have written extensively on having social anxiety. When my JN article came out, i actually felt very anxious at first and wanted to hide away. Mental health stigma is still present in my community and I felt scared. But I needn’t have worried as the reaction has been very positive!

I am still processing all thats going on and I am lucky to have a really good therapist and family/ boyfriend support network to help me deal with the changes going on. I am still adjusting to the financial side of being a freelance writer and pitching to editors at different places. My latest Metro article on child grief came out on Friday and you can read it here: http://metro.co.uk/2018/02/02/children-often-get-sidelined-when-a-family-experiences-loss-why-its-important-we-talk-to-pupils-in-schools-about-grief-7270002/
Over the weekend, I went with my Dad to Iasi, Romania (on the border with Moldova) which is where my great Grandpa and his family were from. It was an eye opening trip- the city is grand and full of culture. However, as Jews we had relatives who died in the Holocaust and found this out using the Yad Vashem Holocaust database when we came back. It was great seeing Iasi but also sad as some of our relatives were taken from there to be killed – but an eye opening trip.
Today, I am feeling thankful and grateful for all thats going on and thankful for you who are reading and following and commenting- and enjoying my work.
With love, Eleanor x

(image: Channel 4)
Channel 4 to launch Lloyds Bank’s £1m award-winning Diversity in Advertising campaign
Lloyds Bank’s winning ad campaign of the Channel 4 £1m Diversity in Advertising Award launches exclusively on Channel 4 on mental health awareness Time To Talk Day (1.2.18).
The adverts will feature celebrities – including Professor Green, Jeremy Paxman, Rachel Riley and Alex Brooker – as well as members of the public and Lloyds Bank colleagues playing a variation of the ‘Who am I?’ sticky-note guessing game, to explore the common misconceptions about living with a non-visible disability.
And to coincide with the campaign’s launch, a new Lloyds Bank and Mental Health UK survey, reveals that although improvements have been made in how society thinks about mental health, 75 per cent of people still think there is a stigma attached to the issue.
Lloyds Bank and creative agency, adam&eveDDB, created the mental health adverts after winning Channel 4’s Diversity in Advertising Award, set up by the broadcaster to improve diversity in advertising.
As the award winner, Lloyds Bank will receive £1m worth of advertising airtime on Channel 4. The competition invited entrants to put forward creative ideas featuring non-visible disabilities.
Channel 4’s Sales Director Jonathan Allan said: “Producing an advert that puts non-visible disabilities at its heart was a demanding brief and it’s been a real pleasure working with Lloyds and adamandeveddb as they developed a fantastic new campaign that makes people think more profoundly about mental health.
“If this campaign can encourage the public and advertisers to think a little harder about all aspects of diversity, it can help make a real difference to people’s lives.”
“The TV ad is brilliantly simple, yet hugely effective,” says Robin Bulloch, Managing Director, Lloyds Bank. “And while winning the Channel 4 Annual Diversity in Advertising Award in itself is a great achievement, the positive difference the campaign will hopefully allow us to make to so many people’s lives is the real ambition here. By raising awareness of invisible disabilities and taking action to promote healthy wellbeing, we can support our colleagues to recognise the signs and feel confident and equipped to support customers and each other.”
Lloyds Bank has been working with Mental Health UK to launch #GetTheInsideOut which will appear on the adverts. #GetTheInsideOut campaign will encourage more people to speak about mental health and aims to inspire those living with a condition to speak up about mental health.
Research from Lloyds Bank and Mental Health UK, undertaken by YouGov, found that seventy-five per cent of respondents feel there is a stigma in Britain attached to people with mental health conditions. And 88 per cent feel society needs to do more (much more (62%) or a little more (25%)) to better understand mental health issues.
The survey reveals that 67 per cent of respondents think people are more comfortable talking about mental health conditions now than they were five years ago. And people feel that the four main factors behind this change were – celebrities talking about mental health (70 per cent); media stories about mental health (70 per cent); societal change (68 per cent); and charities raising awareness (56 per cent).
But the research also reveals that 74 per cent of respondents think people would be fairly unwilling (62 per cent) or not willing at all (11 per cent), to discuss their own mental health issues.
Managing Director of Mental Health UK Brian Dow welcomed the research commissioned by Lloyds Bank and said: “We have come a long way in a short time to raise awareness. In large part thanks to the hard work of the charity sector, campaigns like Time to Change, a willingness of celebrities, notably the Royal Family, to talk about mental health and positive engagement by the media.
“Nevertheless this research shows that we cannot rest of on our laurels – there is a lot more that we need to do.”
Although the survey showed that people think significant steps have been made in the past five years on people’s awareness of mental health, more still needs to be done.
The survey discovers that compared to five years ago;
In addition;
Lloyds Bank is proud to be working in partnership with Mental Health UK. Together the Bank and Charity aim to promote awareness of the link between mental health and money problems, encourage discussion between customers and colleagues. To date, colleagues and customers have raised over £4.8 million which has enabled Mental Health UK to design, build and launch a pioneering new service called Mental Health and Money Advice. This service is the UK’s first advice service dedicated to helping people understand, manage and improve their financial and mental health.
For further information –
Channel 4 –
Tim English, Group PR Manager
Lloyds Bank –
Eve Speight
M: 07585965319
E: eve.speight@lloydsbanking.com