
Bipolar disorder (formerly referred to as manic depression) is a condition characterized by mood oscillations- moving between high and low mood. A person suffering from bipolar disorder experiences mood changes and these changes are often erratic and unforeseen.
Symptoms of this disorder regularly change and that is one of the reasons why it can be such a difficult condition to treat and keep a consistent state of mood and activity for sufferers. However, it is possible!
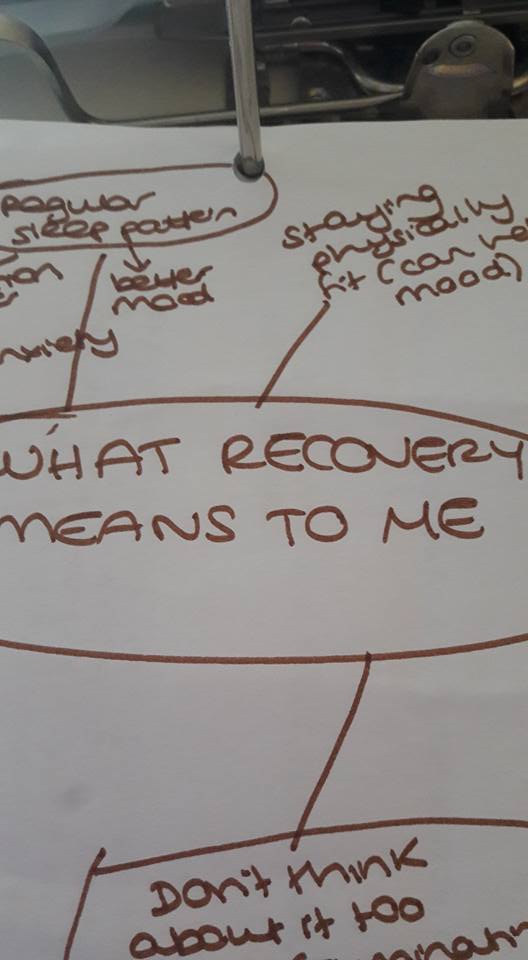
Little things can help and here are 7 tips that might just help make symptoms slightly better:
- Make sure you get the Right Amount of Sleep
People who suffer from bipolar disorder often have erratic sleeping patterns. It is believed that one-quarter of these cases sleep too much at night while about a one-third experience difficulty in falling sleep, thereby suffering from insomnia.
As irregular sleeping patterns may precipitate depressive episodes, experts advise setting up an alarm to ensure one gets up at the same time each morning as well as setting fixed hours for sleep in the evening so that the body can adapt to this necessary function.
- Consistently take your prescribed Medication
According to Cara Hoepner, a nurse practitioner who also has this condition, discipline is the key when it comes to taking medication prescribed for bipolar disorder. However, she also agrees this can be a difficult task, seeing as some of the medications commonly prescribed (such as Lithium) require constant monitoring via blood tests to ensure they do not become harmful to the patient. Lithium can be toxic in rare cases and so its important to work with a good medical team.
Coupled with the fact that skipping medication will often trigger a relapse, she advises that all patients with this condition should exercise diligence and discipline in taking their meds. Tablet boxes can be very helpful for multiple medications.
- Shun Drugs and Alcohol
An expert in bipolar disorder, Bearden, claims that nearly half of patients of bipolar disorder have problems with substance abuse. He also states that this is one of the major reasons why many treatments do not succeed, due to it impeding recovery.
He therefore advises that while alcohol may appear a welcome refuge for bipolar patients in that it temporarily relieves depression, the mere fact that it triggers a depressive state in the brain as well as erratic sleeping patterns and mood oscillations, goes against the purpose. In addition, alcohol and drugs may impair cognitive functioning and hinder chances of recovery- they exacerbate high and low episodes in the condition.
- Invest in Therapy
One of the best ways to improve bipolar disorder symptoms is to invest in therapy, including talking therapies, CBT, art therapy and more. While it may seem unappealing to many patients, therapy actually goes a long way in improving their chances of recovery.
Cognitive behavioural therapy helps patients understand and interpret events and thoughts, thereby enabling them to get back to their normal routine. There are other therapies which assist recovery and maintaining stable relationships .
- Learn the Triggers
Learning the triggers of bipolar disorder may help the patient nip the episode in the bud by actually dealing with these triggers before they develop into a full-blown episode.
Some of the triggers that make people unwell include sleep deprivation, social isolation and stressors eg divorce, death, change or job or having a baby . Other major changes in your life may also trigger depressive or manic tendencies, especially if they disrupt your routine so be careful to look after yourself in times of high stress.
- Learn the Side Effects
The most common side effect of taking Lithium or other anti psychotic medication is metabolic syndrome, a side effect that majorly involves the impairment in the functionality of the kidney and the pancreas. A spectrum of effects such as high cholesterol, insulin resistance and weight gain would ensue, and this is where you need to deal with the to keep optimal health. A healthy diet and exercise is always important.
- Connect with Friends and Family (Support Network)
If you have a good support network, its so important to share how you are feeling with close relations or best friends. By discussing your problems with those you trust, they hopefully will provide the emotional support needed to get through difficulties and help recommend further treatment or come with you to the Doctor.
In a nut shell, do not sit back and let your mood disorder take over without help. Speak out and let your friends and family help you out. In some families, there is a stigma so please do be careful as to who you let in when you are unwell.
Living with bipolar disorder is not an easy experience. However, by understanding how to deal with the symptoms, you can certainly improve your symptoms to keep you healthy and well. Read widely and remember that however debilitating episodes can be, Bipolar can be managed on medication and with therapy and. support. You are not alone.
Marcus regularly blogs at psysci, a psychology, science blog that examines the latest research and explains how findings can impact and improve people’s lives






 .
.