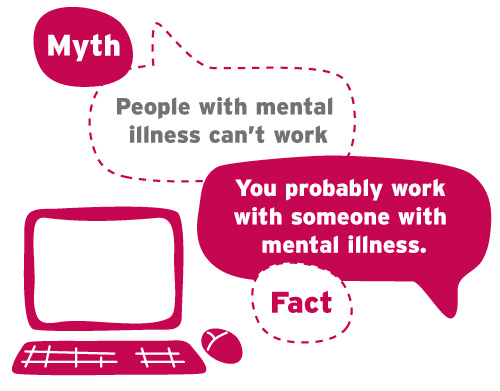
Last year, 916 children per day in the UK were referred to the Child and Adolescent Mental Health Service. In some areas of the UK, there are mental health appointment waiting times of up to 2 years.
As with everything, we need to learn from this, adapt and solve. Many of our children are subject to a huge amount of information through a variety of channels including social media, news, peers etc, much, much more than if you look at only ten years ago. With these added pressures, we need to ensure they have a more robust support system in place that is ready to react when they need it.
Arthur Ellis: School Enterprise is a non-profit organisation solving mental health issues. Founded through the real life experience of Jon Manning who suffers with Bipolar Disorder. With the help from Medical Professionals, Teachers and Local Authorities, AEforSchools was created, a support system that embeds itself in schools and mentors pupils on those waiting lists and provides empowering workshops for those within school counselling.
Like many things, a mental health issue snowballs, it doesn’t always go away, it may get worse. With the numbers rising, our young people need to understand and be able to differentiate between good mental health and mental illness and know how to take control of their lives to minimise the effects of it. The more children that can take this control at a young age, the more resilient they will become and be able to live fuller lives as they grow.
One thing that I have learnt from my journey to gaining a diagnosis, is that a support network is key. You need to be able to feel comfortable enough to open up to someone who can listen and work with you to support you. Not everyone will be able to help with everything. Personally, my Mum and Dad had different approaches, I would approach one for certain things and the other for something else.
Another main task I took on was exercise, no matter how small. Some days, I didn’t feel able , which is okay. I would however, make sure I did three lots of exercise per week. I found that setting an achievable goal helped so much with giving me a purpose, I could relate that back to how I felt after a jog or a few press ups and it began feeling better…with that, I added a day. This sometimes took so long I felt there was no progress at all but I knew the most important thing was that I was doing it. I found that my Mum was the part of my support network to help push me to not to forget those press ups! You tend to do it when a strong, female is telling you to!
Making little goals and having a support network to help push you to strive towards goals is a great way of tackling issues. You may need medical intervention but this is a good way to help without it (or with it depending on what you need). It is easier to stop a snowball rolling down a hill while it’s still small. The further down it gets, the more help you will need- and that is OK. Be open. Those that are close to you often understand, tell someone you trust.
When I first told people about my diagnosis I often got the reaction ‘Well that makes sense’. We had all been thinking the same thing but hadn’t spoken about it. I was shaking at the thought of telling people, not knowing how they would react, what they would say and what they wouldn’t say- but how they might look. However, because it was the right people, it was fine, liberating in fact to disclose my bipolar!
So use that network you have around you, talk about how you’re feeling and think about something you love, do it in small doses and get your network to help you complete those goals.
Teach your children the same and they will grow up more resilient, more confident and able to handle the ups and downs of life.
Jon Manning, Founder, Arthur Ellis: School Enterprise https://www.arthurellisltd.com/
This post was featured by Twinkl in their Mental Health in Schools Blog‘.