(image: Zohr Nemati: Unsplash)
Mental health is an essential part of overall well-being, yet it is often overlooked until symptoms become overwhelming. Millions of people around the world live with mental health conditions that can affect their mood, thoughts, and behavior. These challenges can interfere with relationships, work, and daily routines, but the good news is that treatment options are more accessible and effective today than ever before.
When individuals understand their condition and seek the right support, they can build healthier coping strategies and regain control of their lives. Two common struggles people face are bipolar disorder and anxiety—both of which can be complicated further when substance use is involved. Exploring recovery options designed specifically for these conditions can open the door to long-term healing.
The Importance of Addressing Mental Health Early
Early recognition of mental health symptoms is critical. Too often, individuals dismiss mood swings, prolonged sadness, excessive worry, or fatigue as “just stress” or “a bad week.” However, these patterns can signal a deeper issue that requires professional support. Addressing mental health concerns at the onset not only improves outcomes but can also prevent the development of secondary challenges such as addiction, chronic stress, or physical health problems.
By taking proactive steps, individuals are more likely to develop resilience and maintain stability over time. Family members, friends, and colleagues also play an important role by offering encouragement and understanding instead of judgment or stigma.
Understanding Bipolar Disorder
Bipolar disorder is one of the most misunderstood mental health conditions. Characterized by extreme shifts in mood, energy, and activity levels, it goes far beyond the typical ups and downs that people experience in daily life. Those with bipolar disorder may experience manic or hypomanic episodes—periods of high energy, impulsivity, and elevated mood—followed by depressive episodes that bring sadness, hopelessness, or loss of interest in activities.
Because bipolar disorder exists on a spectrum, its symptoms vary greatly from person to person. This makes individualized care essential. Professional intervention, therapy, and medical management can significantly reduce the intensity and frequency of mood episodes, allowing individuals to lead fulfilling and balanced lives.
For those seeking guidance, comprehensive Bipolar Disorder Treatment programs provide structured support that combines psychotherapy, medication management, and lifestyle strategies to stabilize mood patterns. These programs focus on helping individuals better understand their triggers, strengthen coping mechanisms, and create long-term wellness plans.
The Overlap Between Mental Health and Substance Use
Mental health conditions often coexist with substance use disorders. This dual challenge, known as co-occurring disorders, can complicate both diagnosis and treatment. For example, individuals with bipolar disorder may use drugs or alcohol during manic episodes to maintain their energy or during depressive episodes to numb emotional pain. Similarly, those with anxiety might turn to substances as a form of temporary relief, leading to dependency over time.
The presence of co-occurring disorders makes it critical to find treatment centers that specialize in dual diagnosis. Traditional approaches that treat mental health and substance use separately may fail to address the underlying causes of each condition, resulting in relapse or incomplete recovery. Integrated treatment programs, on the other hand, provide a holistic approach that tackles both issues simultaneously, improving long-term outcomes.
Anxiety and Its Connection to Addiction
Anxiety disorders are among the most common mental health conditions worldwide. They can manifest as generalized anxiety, panic attacks, social anxiety, or phobias. For many, constant worry and fear interfere with work performance, social interactions, and even physical health.
When anxiety is left untreated, individuals often look for ways to escape their symptoms. Unfortunately, this can lead to reliance on alcohol, prescription medications, or illicit substances. While these may provide short-term relief, they create long-term consequences and increase the risk of developing addiction.
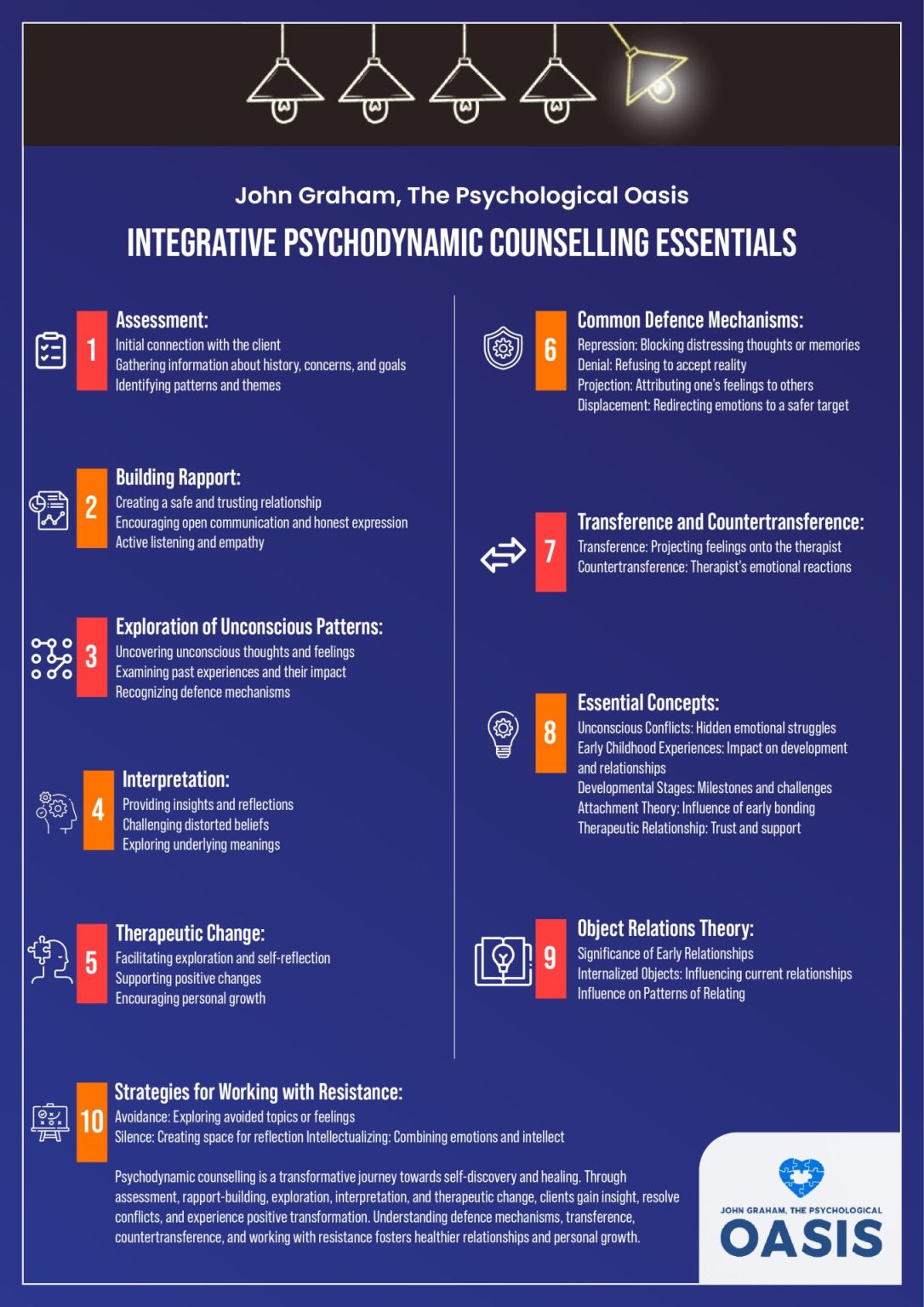
To break this cycle, specialized anxiety and addiction treatment programs are designed to address both issues together. These programs typically combine evidence-based therapies such as cognitive-behavioural therapy (CBT), mindfulness practices, and medical support to help individuals identify the root causes of their anxiety while also treating their substance use.

(image: Sydney Rae: Unsplash)
Building a Strong Support System
Professional treatment is only one piece of the recovery puzzle. Having a strong support network can make a tremendous difference in maintaining long-term wellness. Family therapy, peer support groups, and community-based programs help individuals stay accountable while fostering connections that reduce isolation.
Loved ones can also benefit from education and counseling, as understanding mental health conditions makes it easier to provide the right kind of support. Encouraging open conversations about mental health challenges helps break down stigma and creates an environment where healing is possible.
Healthy Lifestyle and Daily Habits
Lifestyle changes play a critical role in managing conditions like bipolar disorder and anxiety. Regular exercise, balanced nutrition, adequate sleep, and mindfulness practices can all reduce symptom severity. For example, yoga and meditation help regulate stress, while consistent sleep patterns can stabilize mood swings.
Journaling, creative activities, and spending time in nature are additional strategies that promote mental clarity and emotional balance. While these habits may not replace professional care, they work in tandem with treatment to strengthen resilience.
Long-Term Recovery and Hope
Recovery is not a one-time event—it’s an ongoing process that requires commitment, patience, and self-compassion. Relapses or setbacks may occur, but they don’t mean failure. Instead, they can serve as opportunities to re-evaluate strategies and adjust treatment plans.
The growing availability of specialized programs for conditions like bipolar disorder and anxiety shows that no one has to face these challenges alone. With proper care, individuals can achieve stability, rebuild relationships, and pursue meaningful goals.
Final Thoughts
Mental health conditions such as bipolar disorder and anxiety can feel overwhelming, especially when compounded by substance use. However, effective treatment and recovery programs provide hope and healing. By seeking out resources tailored to specific needs, individuals can find balance and create a foundation for lasting well-being. It is important to be lead by a psychiatrist about medication and treatment when someone also has substance abuse.
No matter how challenging the journey may seem, recovery is always possible. Support, understanding, and professional guidance are the keys to moving forward and embracing a healthier, more fulfilling future.
This blog contains sponsored links.