Mood disorders encompass many disorders of how you feel from day-to-day, whether that is abnormally elevated (mania) or depressed and in low mood. They can include depressive illness such as major depressive disorder, dysthymia, postnatal depression and the bipolar spectrum disorders. They also feature anxiety and panic disorders. These are often down to brain chemistry and sometimes environment.
(image: Pinterest/ Healthyplace.com)
Major Depressive Disorder
Major depression is defined as a depressive illness where you experience a significantly lowered mood and a loss of interest in activities that you would normally enjoy. While it is normal to feel sadness and grief when your life significantly changes, such as when a loved one passes away, when it doesn’t go away or gets worse, it may evolve into major depression. Some of the symptoms of depression are:
• Feelings of helplessness or hopelessness • Feeling guilty over insignificant things • Withdrawing from family and friends • Drinking alcohol or taking drugs as a coping mechanism • Having problems with concentration • Being unproductive • Having a lack of confidence • Feeling irritated or frustrated • Having a lack of interest in sex.
While sometimes a depressive episode seems to come out of the blue, there are often things that can trigger them. These may include: Genetic risk factors • Alcohol or other substance abuse • Medical problems such as thyroid issues or chronic pain • Certain medications such as steroids • Sleeping problems • Stressful life events
Studies have shown that there appears to be a genetic component to depression. That is, if one of your parents has a depressive illness, you may end up suffering from depression yourself.
Dysthymia is a chronic form of depression that occurs when you suffer from a mild to moderate depression for at least two years. Although dysthymia causes problems in everyday life, dysthymia is often not severe enough to warrant hospitalisation. The chronic nature of the disorder means that you may believe that you have always felt like this.
The good news is that there are a wide range of medications to treat major depressive disorder, such as antidepressants. There are many kinds of medications around, and you may have to try a few until you and your psychiatrist find the perfect one with little to no side effects.
As of the time of writing, the antidepressants most commonly used are SSRIs and SNRIs (selective serotonin reuptake inhibitors and serotonin-norepinephrine reuptake inhibitors). These refer to the types of neurotransmitters (chemicals in the brain that affect mood, among other things) that they affect.
With antidepressants, it is extremely important not to stop medication all at once, unless there are serious side effects and even then, only under medical advice. This is because of discontinuation syndrome. Simply put, this means that your body gets used to the medication being in your system (different to addiction where you crave the drug) and you experience symptoms such as nausea, dizziness and insomnia, to name a few.
Another important way to treat depression is psychotherapy in one form or another. This can help you by learning coping skills to deal with depressive thoughts and negative thinking, as well as having someone to speak to with complete privacy. There are a few other ways for you to combat depression in adjunct to medications or therapy.
These are: • Maintaining good sleeping habits • Exercising more • Seeking out activities that bring you pleasure • Being around caring and supportive people
Postnatal Depression
Postnatal depression is a depressive illness where a new mother experiences depression in the first few months after giving birth to a child.
Some of the symptoms of postnatal depression include:
• Feeling sad or empty • Lowered self-esteem • Changing appetite (usually a decrease) • A loss of enjoyment in everyday activities • Changes in sleep patterns such as insomnia • Not being able to concentrate • Feeling cut off from the baby • A loss of interest in sex • Feeling ashamed, guilty or inadequate • Withdrawing from family and friends • Mood swings • Thoughts of harming yourself or the baby
There are a number of factors that make postnatal depression more likely. Some of these may include: • A history of depression, especially postnatal depression in the past • If the baby is sick or colicky • If you are in an abusive relationship • If you are suffering from stress • If you have little support from family and friends •
Treatment for postnatal depression is essentially similar to that for major depression, such as antidepressants and therapy and in some cases intervention from a psychiatrist or hospital team is required.
Bipolar Disorder Spectrum
Bipolar disorder is a mental illness characterised by periods of extreme mood states known as mania and depression. It is one of the most serious mental illnesses and is the sixth most disabling condition in the world at the time of writing. It is chronic and potentially life threatening. However, those with it can go on to recovery and live happy and fulfilled lives between episodes.
According to some studies, one in fifty people may suffer from a form of bipolar disorder. In many cases, there is a family history.
Mania is one pole of bipolar disorder – an extremely elevated or depressed mood, sometimes accompanied by psychosis. You may have racing thoughts or speak so quickly it is difficult for others to understand. You may also have trouble getting to sleep at night or suffer from insomnia. There is a danger of reckless behaviour such as overspending, unsafe sexual activity or aggression. You may feel a sense of grandiosity, making unrealistic plans. Despite mania feeling great at the time, the consequences of mania can be destructive.
Some of the signs of depression include a lowered mood, self-esteem or interest in enjoyable activities, pessimism, reduced energy and changes in appetite. Suicidal thoughts are also possible and must be monitored closely. As bipolar disorder is a recurrent illness and there isn’t any known cure, you may need to take medications to maintain your mood at a normal level.
Hypomania is the hallmark of bipolar II where the patient might feel euphoria or agitation. Hypomanic episodes are similar to manic episodes except they are less severe and sometimes pleasurable to you. There is never psychosis in a hypomanic episode. Despite hypomania increasing productivity, or making you feel increased self-esteem, the consequences can be major, especially as your mood goes down to depression.
A mixed state is a combination of manic and depressed symptoms. In a mixed state you may feel very sad or hopeless while feeling extremely energised. These can be dangerous, because of the suicide risk from being depressed as well as impulsive. If you feel you are heading into a mixed state, you should contact your psychiatrist as soon as possible.
Bipolar disorder type I is characterised by at least one episode of full-blown mania as well as depressive episodes. There is also a chance of psychosis (delusions/ hallucinations) accompanying a manic episode. Bipolar type II features only hypomania and never mania or psychosis. While these manias are less destructive, the depression tends to be worse, and there is often a high suicide risk.
Cyclothymia is a bipolar spectrum disorder where you may have long periods of minor depression lasting at least two years alternating with hypomania. These depressive periods tend to be irritable and agitated rather than melancholic and lacking in energy.
Bipolar NOS (not otherwise specified) simply refers to bipolar disorders that do not strictly meet the criteria of any of the previously mentioned types of bipolar disorder.
The treatment of bipolar disorder involves medications such as Lithium carbonate, lamotrigine, sodium valporate, and quetiapine, as well as psychotherapy to help overcome negative thoughts that exacerbate depression or after effects of mania.
As bipolar disorder is a recurrent illness and there isn’t any known cure, you may need to take medications for life to maintain your mood at a normal level. Despite this, many patients continue to do well as long as they stay compliant with treatment and keep aware of their changing mood states.
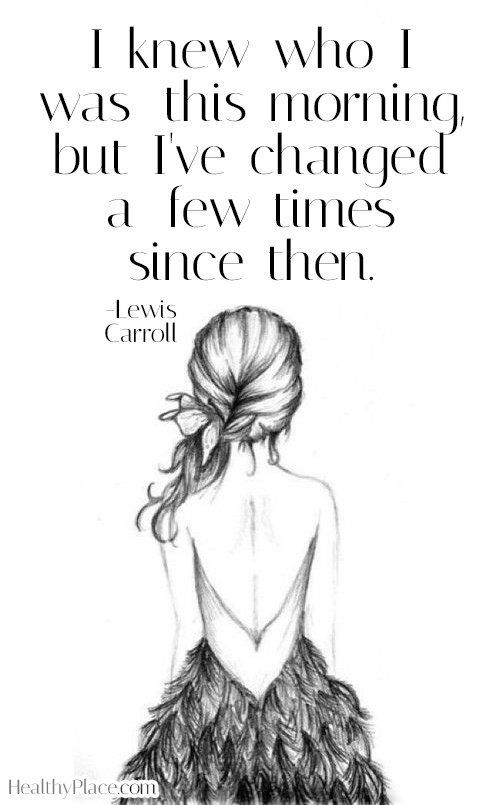
(image: MTVFORA: http://fora.mtv.ca/words-of-wisdom-celebrity-quotes-on-mental-wellness/)
Anxiety Disorders
The term anxiety disorder covers a wide range of illnesses from panic disorder to post-traumatic stress disorder (PTSD). Despite the wide range of diseases, many share similar treatment options. There is a stigma affecting some anxiety disorders due to stereotypes in the media.
Generalised Anxiety Disorder
It is normal for people to feel some anxiety over normal life events such as exams, work problems or family issues. However, when it causes problems in your everyday life or is particularly severe you may have an anxiety disorder. Generalised anxiety disorder involves having irrational fears, such as being afraid harm will come to you or your loved ones, financial issues, health, relationships and work.
Physical symptoms when experiencing anxiety may include: • Light-headedness • Becoming tired easily, or being unable to sleep properly • Feeling tense or restless, or losing your temper easily • Nausea • Shortness of breath • Headaches • Trembling • Muscle tension Treatment generally involves medications or therapy.
Psychological treatments may involve: • Learning relaxation techniques such as muscle relaxing exercises or meditation • Therapy to teach you how to solve problems that cause anxiety with anxiety disorders, psychological treatments are generally more effective than medication, however it can still be useful.
The most common treatments are antidepressants or benzodiazepines such as alprazolam or diazepam. Generally, benzodiazepines shouldn’t be taken long-term, as there is a risk of becoming dependent on them.
Anxiety disorders are relatively common in the population, with statistics that approximately 25% of the people suffer some kind of anxiety disorder that may warrant treatment in their lifetime. Anxiety is treatable, and therapy or medication may minimise the effects on your life and relationships.
Panic Disorder
Panic disorder is a mental health condition where you experience a feeling known as a panic attack recurrently.
Some of the symptoms of a panic attack include: • Shortness of breath • Dizziness or light-headedness • Tightness or pain in the chest • Trembling or shaking • Dry mouth • Muscle tension • Difficulty gathering thoughts or speaking • Tingling fingers or feet • A choking or smothering feeling • Hot or cold flushes • Nausea or butterflies • Blurred vision • Fear of dying, losing control or going mad
When you have panic disorder, you may also worry about the implications of a panic attack such as humiliation or feeling of going crazy.
You may try and flee from the situation hoping the panic attack will stop. Panic disorder is generally treated via therapeutic methods rather than medications. This may involve your doctor teaching you about panic disorder, for example, that a panic attack is distinguishable from other mental illnesses such as other anxiety disorders or psychosis – this is known as psycho education.
A therapist may instruct you not to avoid any situations where a panic attack may occur. This may be unpleasant at first, but slowly you will not feel anxious in the situation. This will help prevent agoraphobia and the disability it causes.
A common treatment for anxiety disorders is CBT – but there are many types too including exposure therapy and talking therapies. They can be incredibly helpful for you to overcome feelings of anxiety.
This guest blog was written by Ellie Willis, an expert in mental health.